Lumeon’s central digital command center for cross-continuum care coordination is perceived as best-in-class by Frost & Sullivan
Market Overview:
Care coordination software refers to software applications that are specifically designed to enable various functions related to managing the care of high-risk and at-risk patients, particularly those with chronic conditions and comorbidities or those transitioning between care settings. Historically, EHR, HIE, data analytics and worklist management platforms were used in silos for loosely coordinating care among disparate health information systems. As a result, significant inefficiencies were reported during referral management, transition of care or post-acute disease management, leading to loss of profitability worth 100s of billions of US dollars for payers and providers.
Since 2015, adoption of pure-play technologies that integrate external and internal HISs to view, download, and transfer patients’ medical history and care plans via the EHR has been accelerated, primarily due to regulatory mandates tied to meaningful use objectives.
Today, the US care coordination market is undergoing transformational changes, owing to the next cycle of regulatory requirements a.k.a the “The Pathway to Success” and “Promoting Interoperability” programs proposed by the Centers for Medicare and Medicaid Services (CMS).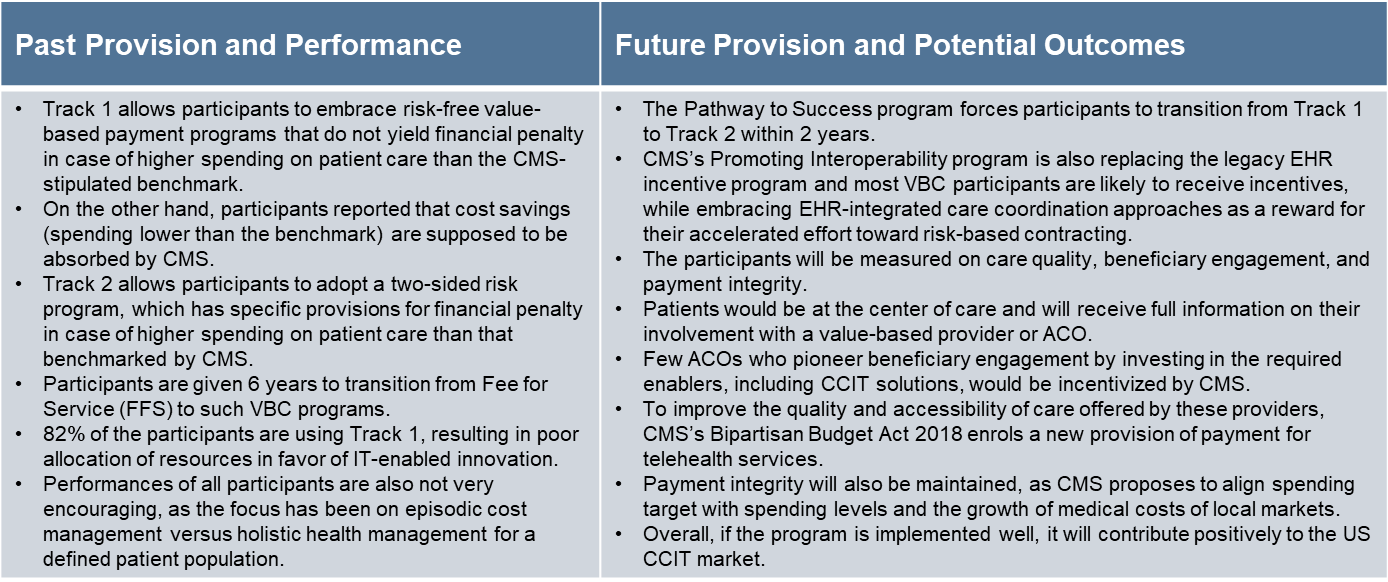
As an outcome of these revolutionary guidelines, all major healthcare stakeholders are embracing next-generation solutions to aid data interoperability, normalization and visualization across the care continuum. Payers, providers, and pharma enterprises are leveraging dedicated care coordination IT (CCIT) and value-added services to facilitate real-time communication between specific care team members, responsible for managing and reporting patient outcomes against various value-based care (VBC) objectives. At the other end, patients and consumers are empowered with information that improves referral management, medication adherence, preventive screening, and routine outreach.
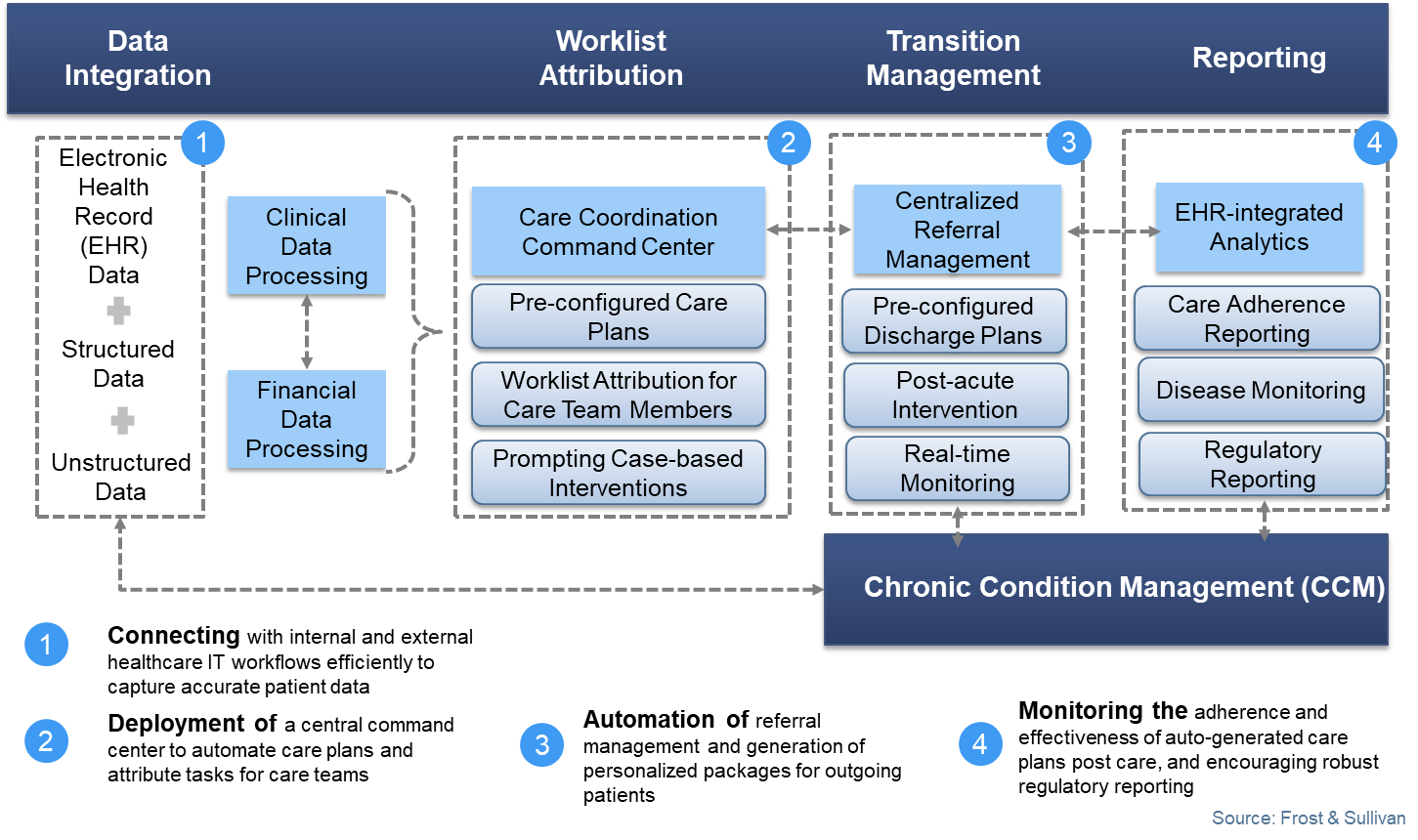
Yet, the US care coordination market is far from being mature. Most providers are still a few years behind, as they are yet to reach the ideal curve where interdisciplinary care coordination can be prompted to aid holistic patient management at a population level. Frost & Sullivan found that 53% of all US-based providers have acknowledged that their care pathways are somewhat coordinated versus 7% that said they are fully coordinated. The handful of providers who demonstrate superior care coordination capabilities are mostly speciality specific health systems and large IDNs that are attributing more than 25% of their net patient revenue to value, quality or risk based payment programs. Frost & Sullivan also reported that these health systems have managed to digitize the entire value chain of patient data management. The common care coordination workflow in action is depicted below.
The ideal care coordination workflow normalizes disparate patient data, triggers automated case-based attribution of tasks among care teams, manages transitional care and aids real-time reporting. Best-in-class providers are expected to launch a central digital command center that will interface with internal EHRs and external referral management systems to create, communicate, update, action and report customized care plans for patients. Frost & Sullivan notes that only a few companies are able to offer these end-to-end care coordination capabilities, and one stands out from the rest.
Company Overview:
Established in 2005 and based in Boston and London, Lumeon is a global healthcare IT company that offers a flagship care pathway management (CPM) solution to a wide range of customers including ambulatory surgical centers, multispecialty hospitals, and large integrated delivery networks.
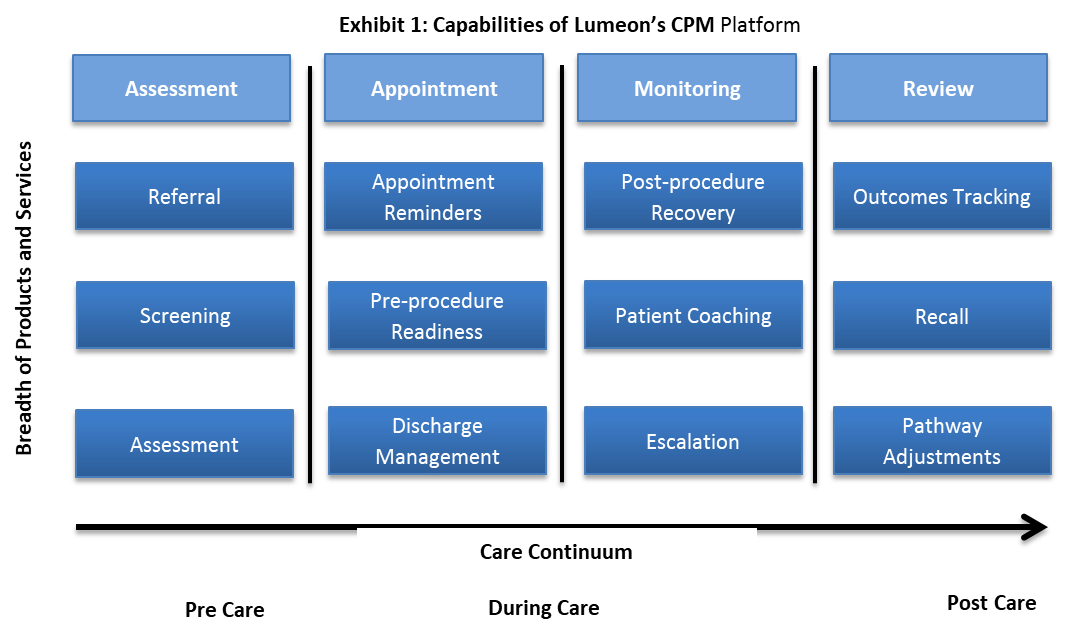
CPM essentially automates the care delivery process by harmonizing disparate patient information across the care continuum, automating care pathway activities accordingly and delivering coordinated insight to care teams that are tasked with standardizing operations, reducing revenue leakages, and maximizing the use of resources for a defined patient population. As patients transition through primary, inpatient, and long-term rehabilitation care, Lumeon helps relevant care teams manage patient referrals and triage; evaluate their eligibilities for appointments; deliver educational materials before and after interventional services; coordinate discharge activities; and initiate automated follow-ups that include personalized goal tracking. By covering the entire patient journey, as Exhibit 1 illustrates, Lumeon estimates that it can increase a health clinics’ operational capacity by as much as 20%, improve patient satisfaction scores by up to 60%, and reduce the cost of patient-related clinical operations by as much as 30%.
Frost & Sullivan’s study further reveals that payers and providers prefer to procure CCIT solutions that are scalable in a patient- and payer-agnostic ecosystem. Industry-leading solutions are capable of seamlessly coordinating care within and outside of hospitals, resulting in deployment of standardized care pathways for both surgical patients and chronic patients. For surgical patients, Lumeon pioneered this approach by empowering customers with an integrated care coordination solution that delivers preoperative readiness support, discharge management and post-surgery recovery education and outcomes tracking. Frost & Sullivan also recognizes that Lumeon’s CPM solutions have increased operational efficiency and reduced manual intervention costs for many health systems across the United States and Europe. Lumeon recently digitized the postnatal care pathway for the Chelsea and Westminster Hospital (CWH) NHS Foundation Trust in the United Kingdom.
All operational and clinical tasks involving postnatal care and discharge are now digitized and visualized on a virtual dashboard that allows a multidisciplinary team of care providers to prioritize interventions for new mothers and babies. As a result, the health system could prevent variability of discharge and reduce mean discharge waiting times to less than 2 hours. CWH also saved more than 1000 bed days a year through improved discharge coordination and liberated resources.
Conclusion:
Frost & Sullivan believes that multi-disciplinary care teams in provider organizations will be the greatest promoters and users of care coordination tools so that they can educate, manage, and monitor patients during care transitions. Patients are also waking up to a new reality of preventive self-care, automated provider engagement, and goal-based recovery management supported by integrated clinical workflows. Lumeon is well positioned to maintain its unique competitive advantage in this market as it caters to these needs and goes beyond to manage personalized intervention plans for complex patient populations across the care continuum.
For its patient-centric platform and unparalleled care coordination capabilities, Lumeon is recognized with Frost & Sullivan’s 2019 Product Line Strategy Leadership Award in the US care coordination IT market.